Healthcare burnout, also known as health worker burnout, remains a pressing challenge for healthcare systems. Burnout among healthcare workers peaked in late 2021 amid the COVID-19 pandemic when more than 60% of clinicians reported symptoms of burnout. This rise in clinician burnout also coincided with over 40% of clinicians reporting intent to leave their organizations or healthcare altogether.
Burnout rates have fallen to near pre-pandemic levels at 46%, but the problem isn’t going away any time soon. The U.S. Department of Health and Human Services Office of the U.S. Surgeon General lists burnout as one of its six priorities (workplace well–being is also listed as a priority, which is related to burnout), stating that “the realities of our health care system are driving many health workers to burnout.”
The consequences of health worker burnout are far and wide, driving up costs for health systems and negatively impacting patient care. By understanding the impacts and causes, health systems can take steps to reduce the risk of burnout in their organizations.
Who is impacted by healthcare burnout?
Burnout impacts everyone in the healthcare matrix, not just clinicians. Its effects are far-reaching and threaten all aspects of healthcare from patient quality to organizational solvency. Here’s how it can affect clinicians, patients and health systems.
How burnout impacts clinicians
The most obvious group affected by health worker burnout is the caregivers themselves. While much of the research on healthcare burnout focuses on physicians, nurses are also experiencing burnout.
According to Medscape’s 2023 report, over 50% of physicians currently report that they are burned out. Nurses are right there with them. According to a May survey conducted by the American Nurses Foundation, 56% of nurses are experiencing burnout, while 64% say they feel “a great deal of stress because of their job.”
Burnout can have devastating impacts on physicians and nurses, affecting their personal lives and careers. Symptoms of health worker burnout can include withdrawal from friends and family, feelings of isolation, depression, departure from the medical field and, in extreme cases, suicide. These symptoms can be tragic on their own, and they can quickly impact a clinician’s ability to deliver quality patient care and can have dire consequences for health systems.
How burnout impacts health systems
When clinicians experience burnout, they are far more likely to leave their organization or healthcare altogether. In one study, physicians who reported an intent to leave due to burnout were three times as likely to have left the organization than those who did not report an intent to leave.
This highlights a unique challenge to the healthcare burnout crisis. Fueled in part by staff shortages and overburdened clinicians, burnout has the potential to lead to more burnout as clinicians leave their organizations or the field altogether.
This turnover (or “burnover“) also places extreme financial strain on health systems, which can, in turn, drive up costs for patients. We will cover the costs of healthcare burnout later in this article.
How healthcare burnout affects patients
As mentioned, patients also feel the effects of healthcare burnout. A page dedicated to health worker burnout on the U.S. Office of the Surgeon General website emphasizes “decreased time spent between provider and patient, increased medical errors and hospital-acquired infections” among the impacts burnout has on patients. Additionally, turnover associated with burnout raises costs for health systems, which in turn can result in higher healthcare costs for patients.
Cost of healthcare burnout
Burnout is putting immense financial pressure on health systems, but placing an exact dollar amount on it is complicated. Conservative, generally accepted estimates suggest that burnout costs the U.S. healthcare system $4.6 billion annually. However, this estimate only accounts for physician turnover and reduced clinical hours attributable to burnout. At an organizational level, it comes out to $7,600 per employed physician each year. In reality, the number is much higher.
A study conducted by the National Bureau of Economic Research in 2023 used data from a midsize healthcare organization with about 500 clinicians to measure the total costs of physician burnout. It discovered that, on average, a burnt-out clinician is less productive than a non-burnt-out counterpart by nearly $81,000 per year. Factoring this in with other considerations, it concluded that the total cost of burnout at this organization likely amounts to over $20 million annually, or $40,000 per employed physician, significantly higher than the commonly accepted estimates.
2018 data from the AMA found that the cost of losing just one physician due to burnout could range from $500,000 to more than $1 million. This estimate includes recruitment, sign-on bonuses, lost billings and onboarding costs.
“The absence of cost calculations for many of the documented impacts of clinician burnout can lead to erroneous decision-making and budgeting by healthcare organizations, such as deciding against implementing a policy that seems too expensive based solely on the cost of turnover when in fact the policy would pass a benefit-cost test based on the full costs burnout.” — NBER, 2023
Again, estimating the exact cost of physician burnout is complex, but any realistic estimation likely puts the costs well into the millions for midsize to large health systems.
While less costly, organizations must also consider the cost of nurse turnover. A study by the National Library of Medicine examined the cost of turnover for nurses at one hospital across three service lines. The cost averaged from $82,000 to $88,000 per nurse lost. It’s important to note that this is only looking at turnover, not the entire cost of burnout. Additionally, turnover can be the result of factors besides just burnout. Nonetheless, the existing data and estimates highlight the extreme financial strain burnout can have on organizations.
What causes burnout in healthcare workers?
Burnout in healthcare has many causes. Societal, cultural, structural and organizational factors all contribute to burnout. Excessive workloads, lack of organizational support and too much time spent on administrative tasks can all contribute to feelings of burnout in clinicians. Let’s take a closer look at how these factors negatively impact clinicians.
Covid-19 pandemic: Of course, the Covid-19 pandemic contributed a great deal to clinician burnout. As we already mentioned, burnout peaked in 2021 during the height of the pandemic. The pandemic intensified what was already a challenging job. Clinicians had to endure long working hours, an overburdened healthcare system, risky working conditions, and a highly politicized public health crisis that at times made for a hostile work environment. However, many of these challenges existed prior to the pandemic.
Overburdened clinicians: One of the leading causes of clinician burnout is excessive workload. Many clinicians simply feel they do not have enough time to deliver quality care and still maintain a work-life balance. Multiple factors contribute to this, but one primary culprit is the amount of time physicians spend on administrative tasks and patient communication rather than patient care.
Most clinicians entered healthcare to care for patients. Increasingly, they are spending less time doing so. A study conducted by JAMIA found that, on average, physicians spend only about 40 percent of their day face-to-face with patients. Much of this is spent on administrative tasks and managing their patient inbox. The AMA features a quote from Dr. CT Lin, CMIO at UCHealth, that sums up how many physicians currently feel:
“Physicians don’t quit their jobs, their patients, or their bosses; they quit their inboxes.” – Dr. CT Lin, CMIO, UCHealth
Staff shortages: Staff shortages are only making matters worse for overburdened clinicians. Studies predict a workforce shortage of more than 195,000 nurses by the year 2031 and up to 180,000 physicians by 2034. According to the AMA, 40% of doctors expressed an interest in leaving their organization within two years.
EHR frustration & tech stress:
EHR frustration, more broadly known as tech stress, is another contributing factor to burnout that has been receiving more attention lately. EHRs and other technologies burden clinicians in multiple ways. First, most clinicians go into healthcare to work with patients, not technology. Thus, the more time they spend interacting with technology, the farther they feel from their mission. But the two factors that are primarily causing EHR-induced burnout are poor usability and the amount of time clinicians spend in the EHR.
Regardless of the chosen EHR, usability is low. One study sought to explore the association between perceived EHR usability and burnout among US physicians. It concluded:
“The usability of current EHR systems received a grade of F by physician users when evaluated using a standardized metric of technology usability. A strong dose-response relationship between EHR usability and the odds of burnout was observed.”
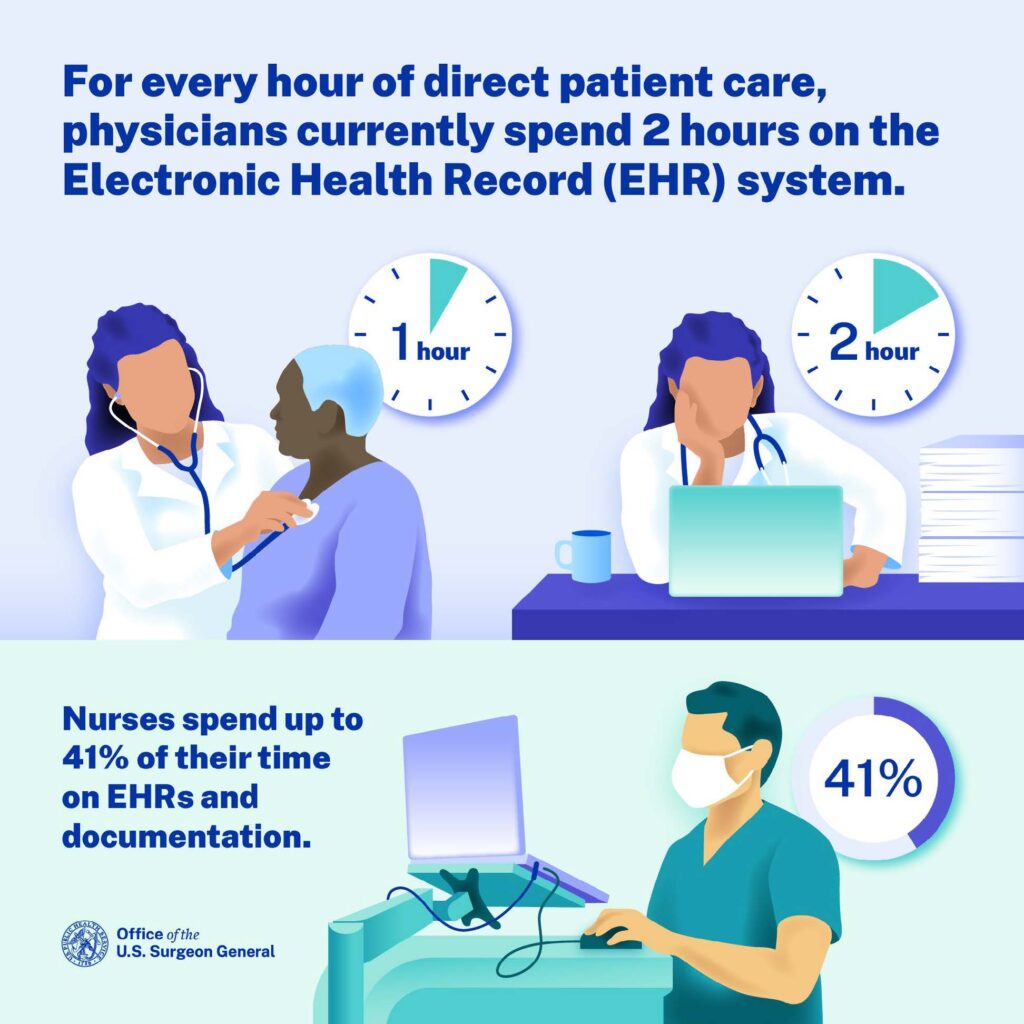
Clinicians are also spending too much time in the EHR. Data from the U.S. Department of Health & Human Services notes that physicians spend two hours in the EHR system for every one hour spent with patients. Nurses spend up to 41% of their time on EHRs and documentation. Streamlining the EHR workflow and allowing clinicians to focus more of their time on patient care is an imperative step in the battle against healthcare burnout.
How to reduce healthcare burnout
There’s no magic button for reducing health worker burnout, but organizations are working toward solutions. Reducing burnout will take a multi-pronged, collaborative effort on behalf of health systems, healthcare vendors, government and more. Here are just some of the strategies that can help reduce burnout in health workers:
AI-aided documentation: Advancements in AI technology allow clinicians to offload some tasks in the EHR, reducing their tech burden. However, some tasks will still likely require a human to complete. AI introduces many opportunities for healthcare, but it also comes with inherent risks.
Virtual care delivery: Virtual nursing is becoming an increasingly popular solution for addressing turnover, staff shortages and offloading tasks for on-the-floor nurses. It allows remote nurses, often those who would otherwise be reaching retirement age, monitor patients and complete administrative tasks, freeing up time for on-site nurses.
Quality initial and ongoing EHR training: One of the best ways to reduce tech stress, a significant contributor to burnout, is by providing clinicians with quality onboarding and ongoing training. Quality training can improve proficiency with the EHR, saving clinicians valuable time in their day-to-day tasks. KLAS Research is on a mission to improve the EHR experience. Data from a study they conducted in 2018 suggests that quality initial training is the single most important determinant in EHR satisfaction, having even more impact on satisfaction than the EHR technology itself.
EHR personalization: Another way to improve the EHR experience is to focus on personalization. EHR personalization is the process of configuring the EHR and its workflows to optimize use for individuals or groups of users. It can make the EHR easier to navigate and more efficient for certain tasks.
Of course, this list is not exhaustive, and the most effective strategies will vary based on the organization and its specific challenges. Other strategies for reducing burnout include increasing wages (particularly for nurses), reducing overall workload, improving organizational culture and involving clinicians in decision-making.
Reducing symptoms of healthcare burnout with uPerform just-in-time training
Reducing healthcare burnout requires a comprehensive strategy. Part of that strategy must be improving EHR usability and satisfaction. uPerform is a just-in-time learning and support platform that enables organizations to create and deliver self-paced learning materials to clinicians directly in their workflow. Leading health systems are leveraging uPerform to scale training efforts and improve EHR satisfaction and proficiency:
- Users of uPerform at Baylor Scott & White Health rate their EHR satisfaction 12.9 points higher than non-users.
- When M Health Fairview embedded a microlearning video in their new eConsent navigator, adoption of the new workflow increased from just 7% to 87%.
- As Aspirus Health grew from a 10-hospital system with 50 clinics to a 17-hospital system with 75 clinics, they were able to leverage uPerform to scale and deliver more training opportunities for end users and improve clinician satisfaction.
Related Articles
Simplify the EHR and battle burnout with uPerform
Looking to simplify and improve the EHR experience for your clinicians as a way to combat burnout? Contact us today to schedule a demo and see how uPerform can guide your users through complex EHR workflows while they work.