Virtual nursing is becoming an increasingly popular solution for health systems facing staffing shortages. Virtual nursing is a form of remote care in which nurses use videoconferencing technology to monitor patients and support bedside nurses.
Spurred by the pandemic, the number of virtual nursing programs in the U.S. increased by 34 percent between 2021 and 2022. The practice is helping many health systems improve the quality of care without the need for more nurses or FTEs.
While virtual nursing offers many benefits, it also poses challenges and requires adequate training and support for the care team. Transitioning to a virtual nursing model requires nurses to learn new workflows, technology and communication skills. A just-in-time training platform like uPerform can help organizations quickly create, scale and deliver the learning opportunities required to facilitate a smooth and successful transition to a virtual nursing model.
What is virtual nursing?
Virtual nursing is a rapidly growing trend in which health systems leverage remote nurses to combat nursing shortages. The specific roles and duties vary by system but usually involve a high-tech workflow that allows remote nurses to monitor and communicate directly with patients or bedside nurses.
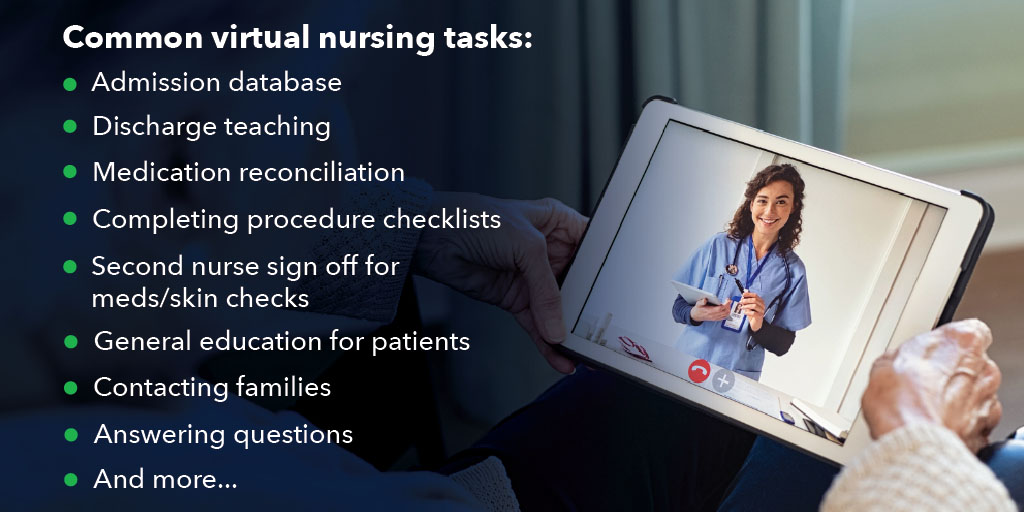
Saint Luke’s Health System of Kansas City began its virtual nursing strategy in 2019. There, remote nurses leverage videoconferencing technology to communicate directly with patients and offload tasks for bedside nurses. This includes tasks such as admission database, discharge teaching, medication reconciliation, completing procedure checklists, second nurse sign off for meds/skin checks, general education for patients, contacting families, answering questions and more. This strategy reduces the need for additional FTEs, helps offload tasks for bedside nurses, and allows remote nurses to respond to patient requests more quickly.
According to Jennifer Ball, director of virtual care at Saint Luke’s, “Patients love the model, because if they just need information, have a question, can’t work their TV, the virtual RUN is just a button push away.”
Virtual nurses can also be a great resource for new nurses, as they can support newer bedside nurses and answer questions, help spot problems or risks before they escalate and offload tasks that can be performed remotely. And with much of the nursing workforce at or approaching retirement age, this form of remote support can be a great way for organizations to retain those nurses who may be considering retirement and tap into their knowledge base.
The Guthrie Clinic leverages its virtual nurses to support bedside nurses. With this strategy, Guthrie has been able to reduce its reliance on traveling nurses by 74 FTEs and reduced labor costs by more than $7 million per year. Guthrie utilizes a high-tech virtual command center, known as the Pulse Center, to monitor patients and support bedside nurses. Their video communication system fully integrates with Epic, allowing virtual nurses to monitor patients and check things like vital signs, ventilator settings and more. On at least one occasion, a virtual nurse has been able to detect concerning patterns in a patient’s vitals and call the rapid response team before the condition escalated.
By leveraging technology, virtual nursing has opened numerous new possibilities for delivering quality healthcare, improving access and managing costs and resources. With its potential to provide faster access to much-needed medical attention, virtual care is set to revolutionize how people receive healthcare in the future.
Leveraging technology to deliver virtual care
Health systems are leveraging a range of new tech solutions to support virtual nursing. Virtual nurses often work in remote centers with high-tech workstations that include multiple monitors, sophisticated dashboards and communication software. Leading EHR platforms like Epic and Cerner have their own modules for supporting remote care, whereas some systems may opt for mounted cameras, speakers, microphones and more basic solutions like Microsoft Teams.
While the technology solutions each health system uses vary, virtual nursing does increase the reliance on technology. It’s important for health systems to consider how tech can impact the daily lives of clinicians, whether positively or negatively. For instance, the increased reliance on Electronic Health Records (EHR) has been noted as a leading cause of clinician burnout. Fortunately, quality initial and ongoing training has been shown to decrease frustration with technology and risks of burnout. Health systems looking to implement virtual nursing models should be prepared to properly train and support nurses in this new role.
Prioritizing education for virtual nurses
The rise of virtual nursing has revolutionized healthcare, making it possible for health systems to extend quality care to more patients amid workforce shortages. However, this new way of delivering care also presents unique challenges that must be addressed to ensure quality standards are met. Education and training for virtual nurses are key in meeting these demands. Virtual nurses must have technical fluency and be able to learn new workflows quickly.
One of the main challenges health systems often face when implementing virtual care is establishing clear communication and workflow guidelines between virtual nurses and bedside nurses. Karen Hughart, senior director of nursing informatics at Vanderbilt University Medical Center, shares some of the early challenges her team encountered after going live with their “virtual sitter” program: “Early on, nursing staff would get frustrated because they felt they either weren’t warned soon enough or they were being interrupted every five minutes to check on patients. It took months of repeated education and meetings to work through ongoing problems.”
Sharing a similar sentiment, Jennifer Ball of Saint Luke’s mentions one of the lessons they learned is “you can never have too much education, training and information shared.”
By prioritizing education for nurses, both virtual and bedside, healthcare organizations can ease any technology burden and ensure their clinicians understand which responsibilities belong to which nursing teams.
Supporting virtual nurses with just-in-time training
A just-in-time training platform like uPerform is a great way to train both bedside and virtual nurses. With just-in-time training, nurses can quickly access help when they need it, allowing them to spend more time on patient care. uPerform also makes it easy to deliver training materials to a geographically dispersed workforce with self-paced and self-guided learning paths that can be accessed wherever and whenever they are needed. Finally, uPerform’s role-based delivery helps ensure virtual nurses see content intended for virtual nurses, whereas bedside nurses may require different materials.
Just-in-time training can also help health systems manage some of the same workforce challenges that they are trying to solve with virtual nursing. For example, on-demand access to workflow training supports less experienced nurses in their daily roles. This can reduce the need to have virtual nurses supporting bedside nurses, allowing those virtual nurses to instead focus on administering patient care.
Clients leveraging uPerform to deliver clinician training have found success in:
- Getting clinicians through initial onboarding and ongoing training faster
- Scaling training opportunities to support organizational growth and new go-lives
- Increasing user adoption of new workflows
- Improving clinician satisfaction with the EHR and training experience
uPerform’s just-in-time training platform makes it easier for organizations to keep nurses informed on necessary information and facilitate a better experience for providers and patients. The ability to deliver highly customized, role-based support at a nurse’s time and place of need – in the workflow – makes uPerform uniquely qualified for supporting a virtual nursing program.
Related Articles
Get started with uPerform today
Want to learn more about how uPerform works with health systems to support clinicians wherever and whenever they need it? Contact us today to schedule a demo and learn how uPerform can work for your organization.