Epic training is the structured education health systems design and deliver to ensure clinicians and staff can use Epic safely, efficiently and consistently. Effective Epic training improves satisfaction, drives proficiency, reduces time spent in the EHR, supports regulatory compliance and maximizes return on investment from Epic implementations and upgrades.
How that training is delivered can lead to vastly different outcomes. This guide provides CMIOs, training leaders, clinical informaticists and L&D teams with an overview of the different types of Epic training and best practices for organizations looking to improve their training models.
What is Epic training in healthcare systems?
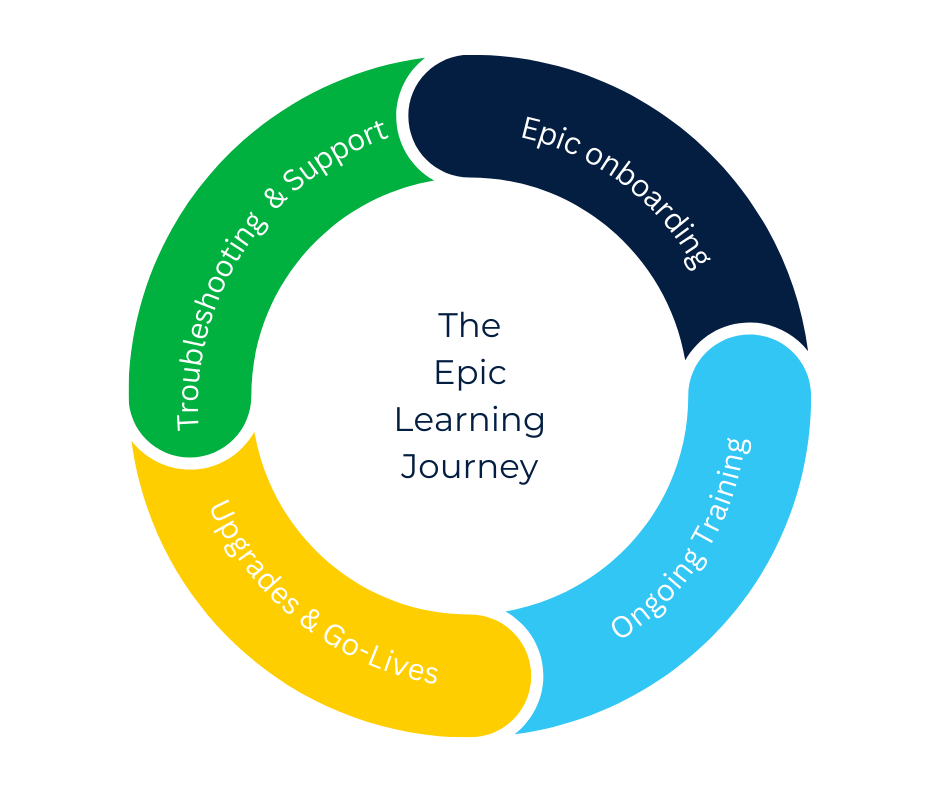
Epic training refers to the structured education health systems provide to ensure clinicians and staff can use Epic effectively, safely and efficiently in their daily workflows. It encompasses the full lifecycle – or Epic learning journey – of learning required to support Epic adoption and optimization, including:
- Onboarding
- Ongoing training
- Upgrade and new go-live training
- Troubleshooting & support
Epic training is the most effective when delivered in various formats, such as classroom instruction, hybrid or virtual training formats and at-the-elbow support.
Why is Epic training so important?
Epic Systems powers modern healthcare with a current US market share of 42% according to a 2024 report by KLAS Research. Epic training helps facilitate:
Patient Safety and Care Quality: Epic drives many aspects of patient care. Clinicians leverage Epic to access patient information, track medical histories, manage treatment plans and more. A thorough understanding of Epic ensures users can deliver quality care to patients.
Productivity and Proficiency: Quality training is the most effective way to drive clinician productivity and proficiency with Epic, saving valuable time that can be redirected to patient care.
Clinician Satisfaction: Healthcare burnout is severely impacting healthcare, and too much time in the EHR is partly to blame. KLAS Research data suggests that quality initial training is the single most important determinant in EHR satisfaction.
Regulatory Compliance: Healthcare organizations must adhere to strict regulatory standards and guidelines. Epic training includes education on compliance requirements, ensuring staff properly maintains things like patient data and security.
Epic Upgrades and Go-Lives: Ongoing Epic training is arguably just as important as initial onboarding. Epic regularly releases upgrades and updates to existing workflows, in addition to releasing new features and applications. Regular ongoing training helps drive adoption of new workflows.
Epic Excellence: Epic is continuously placing more emphasis on Epic training and has built out several recognition programs to promote better use of Epic:
- Epic Good Install Program emphasizes the importance of training and offers a set of best practices and criteria to help organizations through initial implementation and go-live. The program also offers financial incentives for meeting specific criteria.
- Epic Gold Stars is a 10-level initiative designed to promote continuous improvement in EHR usability and feature adoption. Traditionally, the program has assessed a system’s implementation of various Epic tools and modules. Recently, Epic added additional criteria to evaluate a system’s adoption of these tools and modules. While there is no explicit training requirement for the program, health systems are finding that quality workflow-specific training is the most effective strategy for driving adoption.
- Epic Honor Roll offers financial incentives to organizations for effective use and optimization of Epic. The program focuses on eight core components, including key areas like ‘ease of use for providers’ and ‘ease of use for nurses.’
The Epic Learning Journey
Epic training doesn’t end at onboarding. It is a continuous learning journey that evolves as clinicians’ roles, workflows and Epic itself change. A successful Epic training program supports users at every stage of their Epic learning journey.
1. Epic Onboarding
New hires will require Epic training even if they are well-versed in Epic. Because health systems typically customize their Epic instances, workflows and processes will vary at different organizations.
The format, curriculum and length of Epic onboarding can vary greatly by organization, role and training time. For clinical end users (physicians, nurses, MAs, CNAs, etc.), new hire onboarding typically ranges between 6-12 hours. For new implementations, onboarding should include both pre– and post-go-live support per Epic’s recommendations.
Some health systems are exploring new strategies for streamlining onboarding. UCHealth, for example, has adopted a phased onboarding approach – at 30, 60 and 90-day intervals – paired with self-paced virtual onboarding courses. Now new hires hit the floor in as little as 2-3 hours of onboarding.
2. Ongoing Training
Driving engagement with ongoing training is a challenge for many organizations. Delivering in-app training in the workflow can be a great way to drive engagement, guide users through unfamiliar workflows and support users while they work.
3. Upgrades & new go-lives
Epic regularly releases new upgrades, which introduce new workflows and functionality. This can be particularly disruptive when clinicians must relearn processes on-the-fly during patient care, which can lead to frustration, errors and increased calls to the help desk.
An effective Epic training and change communication strategy helps ensure users understand what changes are coming, why it matters and how it affects their daily work. Keeping communications and upgrade training role-based helps improve readership and engagement with learning materials.
4. Troubleshooting & Support
As clinicians encounter unfamiliar scenarios, edge cases or workflow exceptions, they need immediate guidance to resolve issues without disrupting patient care. When support is limited to help desks or is difficult to find, users often rely on workarounds, submit avoidable tickets or experience delays that erode confidence in the system.
Effective Epic training programs embed troubleshooting and support directly into daily workflows through accessible, role-specific guidance. This includes searchable tip sheets, step-by-step walkthroughs and in-application help that enables users to solve problems the moment they occur.
Common Challenges of Traditional Epic Training
Traditional training methods – often centered on classroom instruction or formal eLearning courses – present several limitations when applied at scale. Understanding these challenges and their impacts is the first step in delivering more value with your Epic training.
Limited scalability
Instructor-led training requires significant coordination and staff availability, making it difficult to scale across multiple care sites or geographically dispersed health systems. As organizations onboard new hires or implement frequent Epic upgrades, these models struggle to keep pace without expanding training teams.
High cost and resource demand
Implementing instructor-led training across the enterprise is not only difficult – it’s expensive. It requires instructor time, classroom space, repeated sessions, ongoing content maintenance and time and expenses associated with travel to and from sessions. This format also limits who can participate and when, sometimes restricting new hires’ start dates to whenever the next training can be hosted at their care site.
Low knowledge retention (forgetting curve)
The Ebbinghaus Forgetting Curve shows that learners forget over 55% of what they learn in the first hour after leaving the classroom. When Epic training occurs before clinicians need to apply it, critical workflows are often relearned during patient care rather than retained from training.
Poor learning experience & low satisfaction
Traditional training methods make it difficult to cater to individual learning needs, often leading with a one-size-fits-all approach. Too often, instructor-led training is not role- or workflow-specific. Another challenge with instructor-led training is pacing. Everyone learns at a different pace, which instructor-led training fails to accommodate.
These are just some of the challenges associated with traditional methods of Epic training. Together, they can contribute to a poor learning experience and poor satisfaction with the training experience and Epic itself.
But studies continue to show that clinicians want more training – they just want training that delivers value and minimizes interruption to their daily roles. Modern approaches to training emphasize asynchronous, role-based, and in-workflow learning that reinforces knowledge at the moment of need. By shifting to a just-in-time learning strategy organizations can improve efficiency, scale more effectively, reduce training burden, and better align learning with clinical workflows.
Principles of an effective Epic training program for health systems
Epic training must be able to support users throughout their entire Epic learning journey, while also optimizing organizational resources. To do so, it should be:
Role-based and workflow-specific
Training reflects what users actually do in Epic, not generic system functionality.
Tailored to individual needs
Every user has different learning needs. Offer different learning formats and consider adding test-out options for more experienced Epic users.
Continuous, not event-based
Learning extends beyond onboarding and go-live to support ongoing proficiency and optimization.
Delivered at the moment of need
Users receive guidance when and where they need it – in the workflow.
Scalable and reusable
Training content can be easily updated and reused across roles, departments and upgrades.
Measurable
Programs track not just completion, but proficiency, adoption and impact.
How health systems can build a modern Epic training program
Health systems around the world are reevaluating and reimagining their Epic training strategy to better match the needs of their learners. Here’s what that typically includes:
1. Assess current training assets and gaps
Identify which workflows generate the most questions, errors or support requests and start by prioritizing those.
2. Define role-based learning paths
Map Epic roles to required competencies and workflows and ensure training is workflow specific.
3. Select the right delivery strategy
Determine which mix of classroom instruction, formal eLearning asynchronous or in-workflow learning is best for your organization.
4. Embed training in the workflow
Provide guidance directly in Epic so users can learn while working. This reduces time away from patient care and maximizes knowledge retention.
5. Measure and refine
Use analytics to identify gaps, reinforce learning and continuously improve training effectiveness.
6. Look beyond Epic
When considering how you plan to support your Epic users, consider how that strategy will support other software applications and tools in your tech stack.
Additional training resources on Epic UserWeb
Epic does offer its own training resources on the Epic UserWeb. However, these should be supplementary to a well-rounded training program. Epic’s training resources reflect a Foundations implementation and do not mirror each health system’s specific instance of Epic. That said, these are still good additional resources for organizations looking to improve their Epic training offerings.
Epic WeLearnings provide asynchronous, self-paced eLearning modules focused on Epic fundamentals, workflows and upgrade training.
It’s Possible content delivers microlearning “how-to” content focused on specific tasks and workflows.
Nova Notes provide high-level summaries, explanations of enhancements and guidance on what to expect in workflows affected by upcoming releases.
What’s New: What’s New content highlights recent feature updates, enhancements and new functionality.
Delivering scalable and effective Epic training with uPerform
uPerform’s just-in-time training platform can help organizations build a sustainable Epic training program that drives clinician adoption, proficiency and satisfaction. Health systems leveraging uPerform to deliver just-in-time training report:
Better scalability: As organizations grow, it can be difficult to keep up with increased training demands. uPerform centralizes all your learning content and allows you to scale self-directed learning opportunities to all your Epic users. For instance, Baylor Scott & White Health used uPerform to deliver training to a geographically dispersed user base, saving the organization 186,000 hours of travel and onboarding time.
Faster onboarding: Delivering a self-directed onboarding experience allows organizations to onboarding new hires faster. Emplify Health (Gundersen) has reduced the time it takes to onboard some roles by as much as 75%
Improved Satisfaction: With workflow-specific training available at their time of need, users of uPerform report higher satisfaction with training and Epic than non-users. At M Health Fairview, uPerform users rated their Net EHR Experience Score 19 points higher than non-uPerform users.
Reduced training costs: In-person training is time-consuming and cost prohibitive. uPerform enables organizations to quickly create learning content and deliver it to their entire Epic user base. Without the need for in-person classroom training, organizations save on physical space and travel costs. In 2024, UCHealth credited $3 million in savings to its asynchronous training program.
Related Articles
Create and deliver Epic training with uPerform
uPerform’s just-in-time training and support platform enables training teams to quickly create training materials and deliver them to users based on their role and workflow. Schedule a demo today and learn how uPerform can help you scale your training, improve clinician satisfaction with Epic and drive user proficiency.